CASE 3: Revision of an infected hip implant with pelvic discontinuity, using a custom triflange cup
The Story
“Tanveet had suffered from developmental dysplasia of the hip as a child, leaving her with a fused left hip joint. At the age of 51, this was converted to a left total hip replacement, however this left her with significant pain. Post-operatively she suffered from dislocations and an E. Coli positive wound infection, leaving her unable to weight bear or work. She first came to me to try and help treat the pain.
Prior to her THR, she was fit and well, working and fully independent when mobilising. She had no other medical issues. We had to get to the bottom of what was causing this ongoing pain, so Tanveet could get her life back on the road.”
The Investigation
On clinical examination there was evidence of scaring around the left hip (both a posterior and an anterior approach scar was present). There was some puckering of the skin around the scar suggestive of long-term infection and delayed closure. On movement, she had no remaining abductor strength on the left hand side and mobilised with the difficulty using two crutches. Her left leg was also shortened by approximately 3cm.
We used our first line investigations for painful hip replacements:
Blood inflammatory markers
CRP of 44 mg/L and ESR of 76 off antibiotics - Both markedly raised
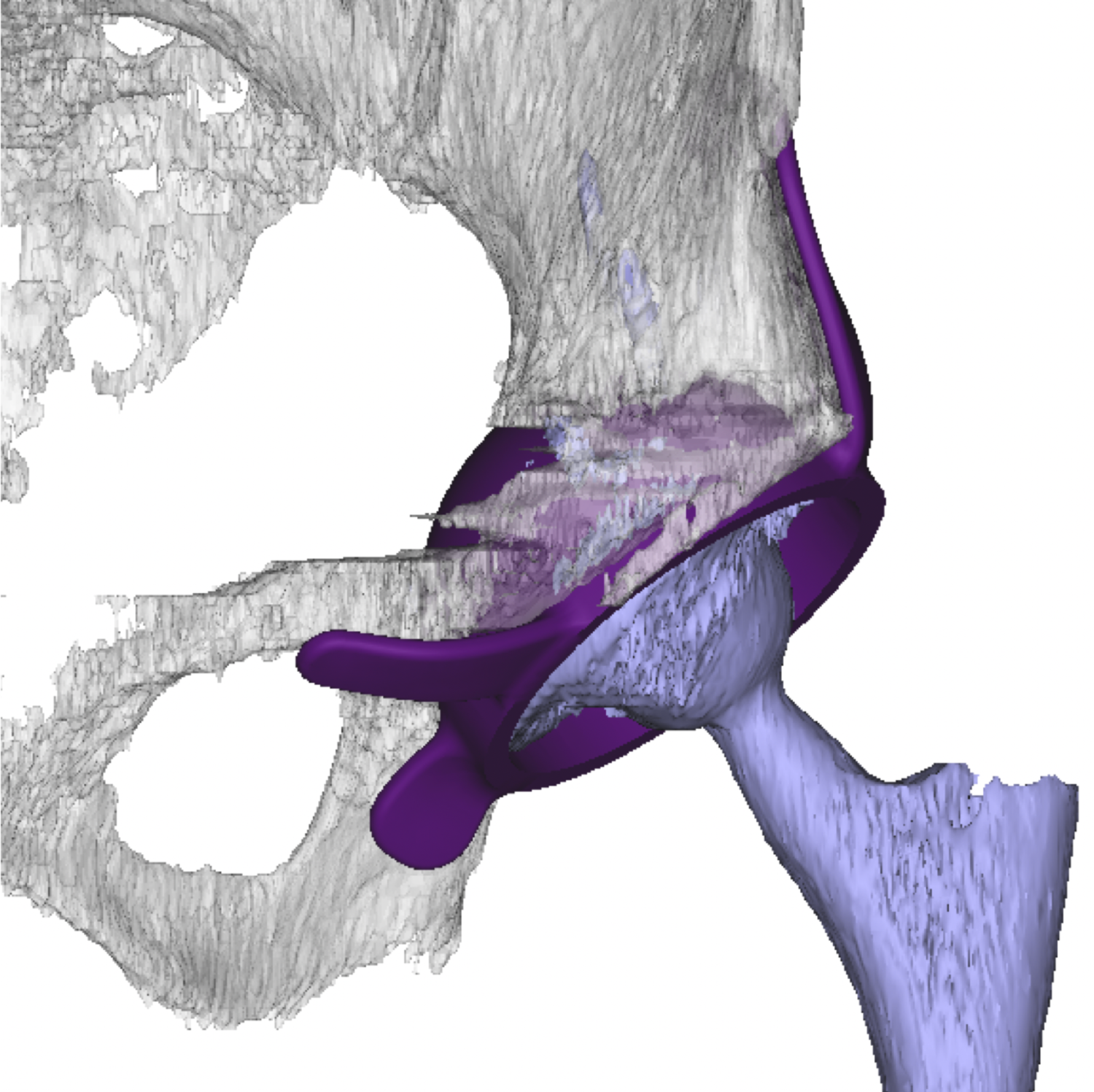
CT scan to assess the 3D pelvic anatomy (and use for generating a custom acetabulum) and the presence of pelvic discontinuity.
Our second line investigations were:
US guided hip aspiration (two weeks after stopping antibiotics)
There was a dry tap
However, the clinical assessment and raised CRP and ESR strongly suggested infection.
The Evidence
Anteroposterior plain radiograph demonstrated an uncemented left hip replacement with evidence of a subtrochanteric osteotomy. A fracture of the pelvic floor is present which has not healed.
3D CT reconstruction further helped to characterise the bony pelvis surrounding the implant. Despite the metal artefact, the CT demonstrated pelvic discontinuity.
The Diagnosis
Tanveet was diagnosed with a painful and infected left total hip replacement further complicated by pelvic discontinuity.
The Plan
Due to the underlying infection, we planned to perform a two-stage revision procedure as advised by our local MDT proceedings. For the first stage we aimed to use a space with cement containing antibiotic to resolve the infection. We used inflammatory markers to guide us as to the timing of the second stage. For the second stage, we planned to use a custom CAD-CAM multi-flange acetabulum designed specifically for this patient. This allowed us to restore the stability of the bony pelvis. We planned to revise the femur with a proximal femoral replacement.
Planning image produced from the pre-operative CT demonstrating the design of the custom multiflange cup
The Operation
First stage revision: We operated through the old incision and used 2 stay sutures to protect the surrounding soft tissues. Five samples were sent for microbiology to confirm the infection and guide antibiotic therapy. The old femoral implant was removed. The remaining femur was reamed to 16mm to accomodate a METS total proximal femoral replacement. The acetabular socket removed with explant and a Magnum 58mm +4mm head was used to achieve stability. Vancomycin infused cement was used to treat the infection locally. At the end of the procedure, the joint was stable and it was closed with vicryl.
Second stage revision: Once again the old incision was used and cultures were sent. The acetabular socket was reamed to 66mm. A custom flanged cup was then implanted with multiple screws. A metal shell was cemented into the custom cup. This construct was stable with a bipolar head and the incision was closed with vicryl.
The Outcome
Anteroposterior plain radiograph taken after the first stage of Tanveet’s treatment. This demonstrates a cemented spacer in situ with a large METS head. Note the staples.
Anteroposterior plain radiograph taken immediately after the second stage of Tanveet’s procedure. The new CAD-CAM flanged cup is in situ and is being used to maintain pelvic stability as well as provide a new acetabulum. Multiple screws have been used to achieve a solid initial fixation.
Anteroposterior plain radiograph taken three and a half years after the second stage of Tanveet’s reconstruction. The acetabular construct remains stable.
The Verdict
“Tanveet returned to my clinic eight weeks after the second stage of her major reconstruction. The wound had healed nicely and she was able to straight leg raise and flex her hip to 90-degrees. She was relieved to have a sense of stability in her left hip. At this point she was advised to start to partially weight bear and wean off of the abduction brace.
At six months post-op, Tanveet was back on her feet, mobilising with the aid of two crutches. She was very happy with the outcome of the operation.”
-
The Paprosky classification system for periacetabular defects is widely recognised and provides a basis for implant selection. Paprosky 3B defects are the most severe and are characterised by supporting bone loss greater than 60% and significant superior-medial migration of the hip centre of rotation (CoR). Traditionally antiprotrusio cages, spanning the ischium and ilium, have been the preferred devices used for the management of Paprosky 3B defects. However, their use is associated with high (29%) rates of failure.
-
-
Please other cases of 3D printed custom acetabular implants such as Case 25.